Aesthetic medicine has entered an era of precision and safety driven by real-time imaging. High-frequency ultrasound (HFUS) is now a powerful adjunct in cosmetic procedures, enabling us to “see” beneath the skin. As experts note, ultrasound has multiple applications in aesthetics – from identifying filler placement to guiding injections and diagnosing complications. Indeed, ultrasound provides unmatched resolution, anatomical detail and blood-flow visualization, making it “a must for managing aesthetic patients”. By mapping facial vessels and tissues live, ultrasound transforms the injector’s awareness of anatomy from static to dynamic, markedly enhancing both safety and accuracy.
Clinically, we use ultrasound before, during and after treatments. Before injections, HFUS scans the target area for major vessels and filler remnants, allowing arterial “roadmaps” that help avoid occlusion. During treatment, a live ultrasound view confirms safe needle or cannula placement. After injection, ultrasound can verify that the product is in the intended plane and that surrounding vessels remain patent. practitioners can visualize the exact depth and location of the needle tip relative to both the desired tissue layers and nearby arteries. This direct feedback shifts filler injections from guesswork to precision, significantly reducing the risk of serious complications such as skin necrosis or vision loss.

Ultrasound’s impact is perhaps best demonstrated in filler treatments. Hyaluronic acid (HA) is the workhorse of soft-tissue augmentation, but even HA carries risks if placed incorrectly. By scanning the treatment area, we can map superficial and deep arterial branches and confirm “safe zones” before inserting the needle. This practice preemptively avoids intravascular injection or compressive occlusion. Importantly, ultrasound also visualizes filler after it’s injected. We can immediately confirm that HA has filled the intended space (often seen as an anechoic cushion) and that surrounding vessel flow is intact. In cases where filler was unknowingly injected into an artery, Doppler ultrasound can localize the obstruction. In short, ultrasound can detect filler material in real time and differentiate it from normal anatomy or pathology.
As one review explains, HA filler shows up as a well-defined black (anechoic) region on ultrasound, whereas products like calcium hydroxyapatite (a collagen stimulator) appear as a cloudier echo with bright particles. This ability to identify the filler type by sonographic pattern is clinically useful for both planning and troubleshooting. For example, if a patient has lumps from past treatments, ultrasound helps determine whether those nodules are HA gel (fluid-like) or a semi-permanent biostimulator (solid microparticles). Knowing the difference guides management: HA can be dissolved with hyaluronidase, whereas CaHA or
PLLA (poly-L-lactic acid) nodules might require other approaches.
The labeling for PLLA (Sculptra) even notes that its microparticles “may be visible … on ultrasound”. In practice, we inform patients that these products can persist in tissue imaging for months. While we don’t routinely ultrasound every biostimulator injection, in any case of unexpected volume or nodule formation, an HFUS scan is invaluable for diagnosis.
Educational Value: For clinicians, ultrasound is also an exceptional teaching tool. Studies describe how using ultrasound before and after filler treatments provides feedback that refines technique. By comparing intended injection plans with actual filler location on imaging, injectors learn from each case and continuously improve their accuracy. This feedback loop promotes an ethical standard of care, as we are no longer “flying blind” but instead using technology to ensure optimal outcomes.
Ultrasound is equally beneficial when injecting neurotoxins like Botox (Botulinum toxin A). Although many toxin injections rely on surface anatomy, certain areas (masseters, neck bands, deep facial muscles) can be challenging. Ultrasound lets us visualize muscle thickness and course, avoiding nearby glands and nerves. For example, guidance in the masseter muscle – commonly treated for hypertrophy or bruxism – improves precision. A recent review of masseter Botox noted that ultrasound guidance significantly increases injection accuracy versus blind technique. The authors emphasize that seeing the muscle in real time reduces risks (like injecting too superficially or missing a muscle head) and enhances patient safety .


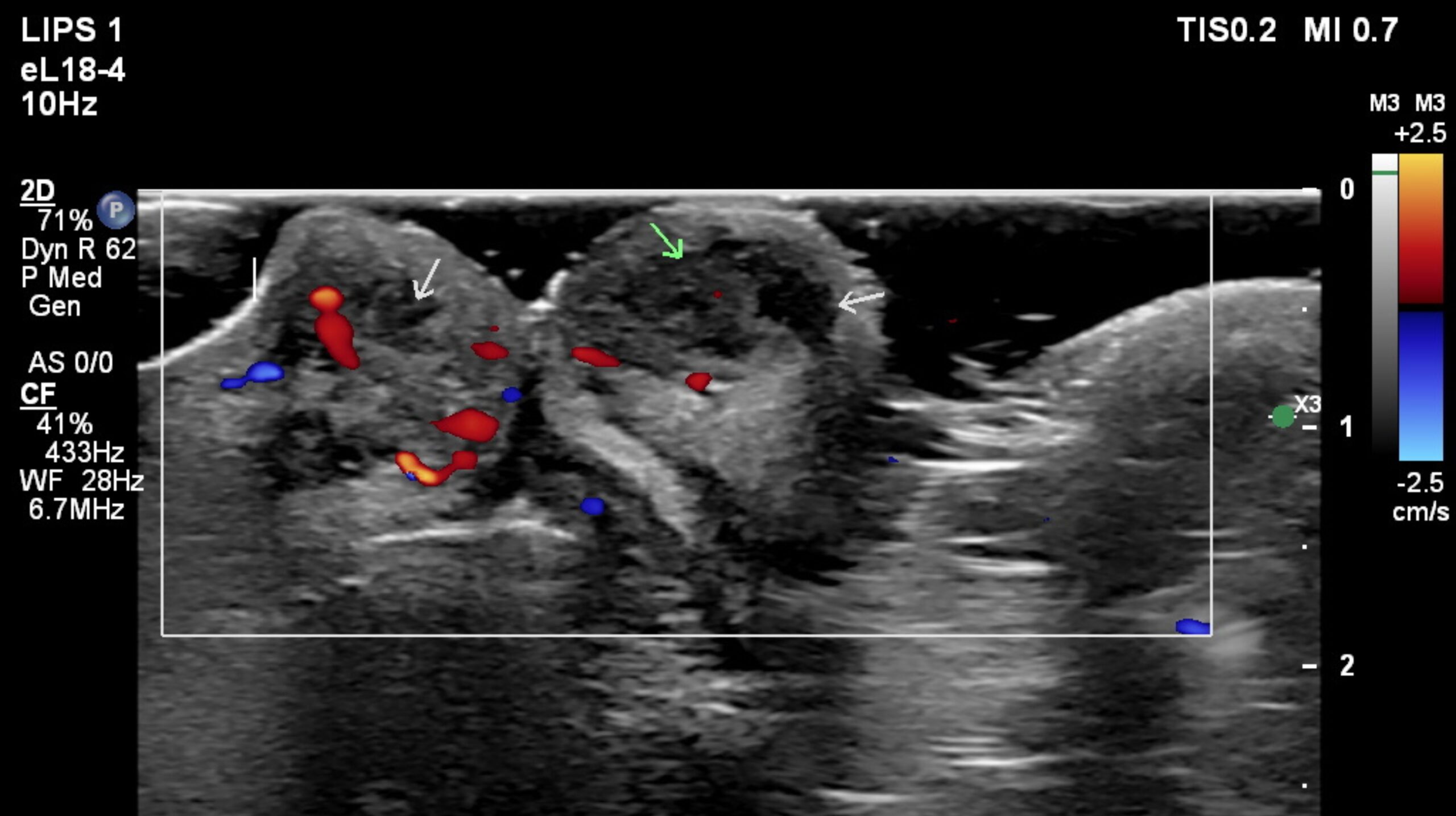
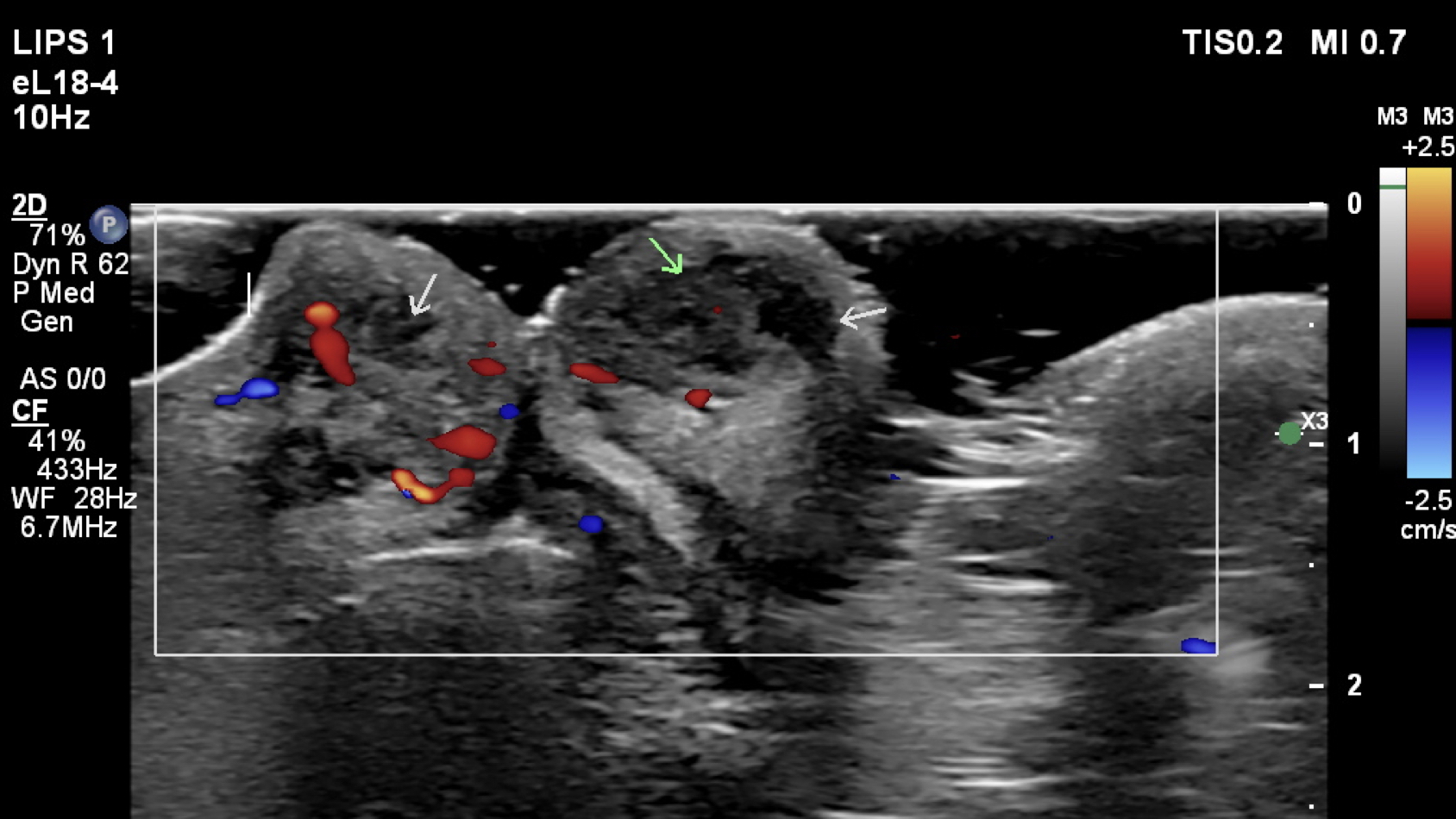
Such imaging is especially helpful in anatomically complex zones (e.g. glabella or jawline). For instance, ultrasound can identify the exact plane of the superficial head of the masseter (see Figure above) and distinguish it from adjacent muscles like risorius or the parotid gland. This avoids “paradoxical bulging” (unwanted asymmetry) or injecting into facial nerve branches. In practice, we often prepare patients for toxin by scanning – marking injection sites on the skin based on the live image.
Injectables for local fat reduction (e.g. deoxycholic acid formulations) have become popular for double-chin or body contouring. Ultrasound can improve these treatments too. Before injecting, we measure subcutaneous fat thickness and locate critical structures (nerves, vessels, glands). This ensures that fat- dissolving enzyme is placed precisely in the adipose layer, not in muscle or under deep fascia. During treatment, we can observe the injected area on ultrasound to confirm even spread of product. After treatment, serial scans objectively track fat reduction.
Research supports these uses. In a study of knee fat injections, ultrasound guidance was integral: the injector used HFUS to monitor subcutaneous thickness and administer deoxycholic acid safely. Patients showed volume reduction in most cases. The authors concluded that ultrasonography “proved to be a useful method to monitor the procedure (correct administration of the preparation) and to assess treatment outcomes”. Another report noted that HFUS was “highly useful in planning, monitoring and treatment outcome assessment” and likely helped reduce complications. In our practice, we similarly find that ultrasound delineates fat layers clearly, guiding the needle to the right depth, and reducing post- injection bruising or irregularity.
Ultrasound is indispensable for early detection and management of complications. The most feared complication is vascular occlusion from intravascular filler injection.
Even with meticulous technique, accidents can happen. Here ultrasound is literally lifesaving.
As soon as a patient reports disproportionate pain or paleness, we can scan the area. Doppler ultrasound rapidly identifies blocked arteries or compromised flow. Once we locate the embolized filler, we perform ultrasound-guided hyaluronidase injection directly into the affected bolus.
In a recent case series, practitioners used ultrasound to precisely localize the culprit filler and injected very low doses of hyaluronidase exactly where needed. All patients recovered fully with minimal enzyme, and no additional tissue damage. As the authors report, “if the lesion at the origin of the skin damage is precisely localized with ultrasound … a few units of hyaluronidase, injected directly into the HA accumulation, effectively resolve the skin damage”. In other words, ultrasound targeting allows us to use far less enzyme and avoid systemic side effects.
Larger studies reinforce this success. In a series of 10 vascular-occlusion cases treated with ultrasound- guided hyaluronidase, all patients had restoration of blood flow on Doppler after treatment. Ultrasound allowed the team to inject up to 750 IU of hyaluronidase while monitoring the vessels in real time; afterward, 100% of arteries and veins were patent again.
Beyond occlusion, ultrasound also helps manage nodules, lumps and granulomas. We can distinguish solid versus fluid collections, guide steroid injections into granulomas, or plan any needed surgical revision. Even in non-acute settings, HFUS can evaluate “silent” issues – for example, an unexplained contour irregularity might be a migrated filler pocket, easily confirmed and measured under ultrasound. These capabilities underscore why experts have called vascular occlusion “the most concerning complication” of fillers and why ultrasound guidance is now considered best practice to prevent it.

With these advanced tools comes professional responsibility. Ultrasound is only as reliable as the operator’s skill. Clinicians must have thorough anatomy training and practical HFUS experience. We emphasize that any ultrasound-guided procedure should only be done by providers certified in both aesthetics and point-of- care ultrasound. In line with Dr. Iman Itani and others, we view ultrasound as an extension of the aesthetic “standard of care”. Just as we wouldn’t inject fillers without understanding facial layers, we should not claim to use ultrasound unless we can accurately interpret the images.
This requires ongoing education. Lueur Clinic encourages practitioners to attend dedicated facial ultrasound workshops (given by leaders like Itani, Schelke and Cavallieri) and to review the literature on sonographic anatomy. Ethically, we should disclose to patients that we are using this technology – it adds time and cost – with the goal of maximizing their safety. In our hands, using ultrasound reflects our commitment to transparency and excellence. Patients often appreciate seeing the scan and understanding exactly what we’re avoiding or targeting.
Ultrasound-guided techniques are transforming aesthetic practice from art back into medicine. By providing a live map of individual anatomy, ultrasound empowers us to tailor each injection with unprecedented care. Across HA fillers, collagen biostimulators, neurotoxins and fat-reduction treatments, the evidence is clear: ultrasound improves accuracy, educates both patient and provider, and greatly reduces the risk of adverse events. Embracing ultrasound is not just an innovation but an ethical imperative for safety-minded clinicians.
In sum, ultrasound makes good aesthetic sense. It blends imaging science with the artistry of rejuvenation – enhancing results and, above all, putting patient safety first.
This article is Medically reviewed by : Dr. Iman Itani MBBS.GP. Aesthetic doctor.
